Cystic Fibrosis Awareness Month 2023
Action, Solidarity, and on Building a Better World for Everybody with CF and Our Families

Intro
Hi, all. Thanks for taking the time to click on this essay on cystic fibrosis awareness month. It’s one of the most important things I’ve ever written. There are multiple audiences and goals for this essay. This essay is in some ways an ode to the global community of people with CF, a community of people that may disagree on some things, but share a rare understanding of what it’s like to live a life filled with frustrations and health consequences due to a microscopic defect. I love this community. I have found a deeper connection to what it means to be alive and part of something bigger and more meaningful because of this community. I despise the suffering cystic fibrosis can cause, but I believe our community proves that compassion and community can outpace suffering.
It’s also an essay that describes how while our community is connected by CF, the interconnectivity does not end there. We are interconnected through a web of connections with our families and friends who have become advocates themselves; we’re connected to the web of advocates, scientists, clinicians, and healthcare professionals who have committed their lives to CF despite often never knowing somebody with CF; we’re connected to the other communities of people with rare and chronic diseases or disabilities who also need advocacy.
Ultimately, this is an essay on solidarity and action because awareness itself won’t be enough to create the better world we all deserve.
As I mentioned, this essay is for multiple audiences so I want to describe the outline and draw attention to a few things. I’m not trying to capture what CF looks like for every single person with the condition. That’s not possible. What I am trying to capture, however, is how nuanced and complex this disease is, which then underscores the need for collective, broad-facing action. To accomplish this, I first describe the point of awareness months and share some thoughts on solidarity. I invite everybody to read these portions (and please share your thoughts, whether you agree, disagree, or just want to contribute to the conversation, directly to me or in the comments below). After, I get into what cystic fibrosis is and some basics on how it’s treated, as well as what the future of CF looks like. This does not cover everybody’s experience, but what it does do is display just how many ways CF affects our bodies and how much goes into creating stability in our lives.
Finally, I get into the ways you can do your part to support our community: Organizations you can support and Congressional actions that are of particular importance to our community (that you can help advocate for).
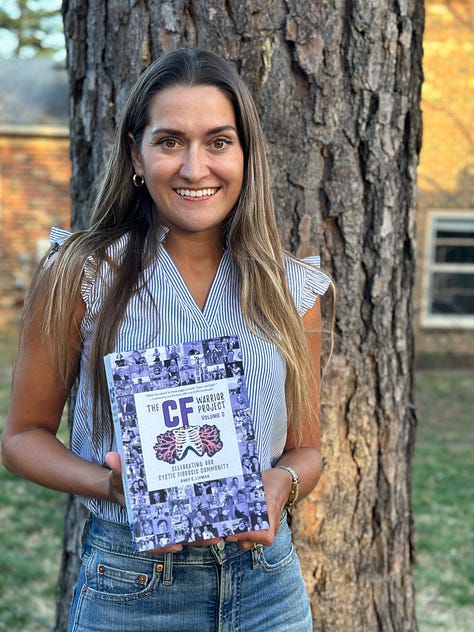
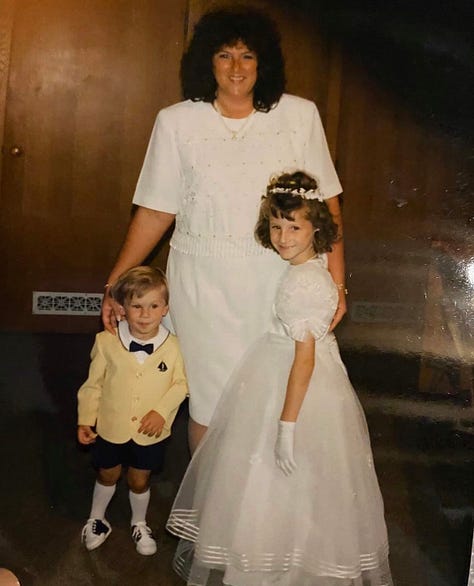
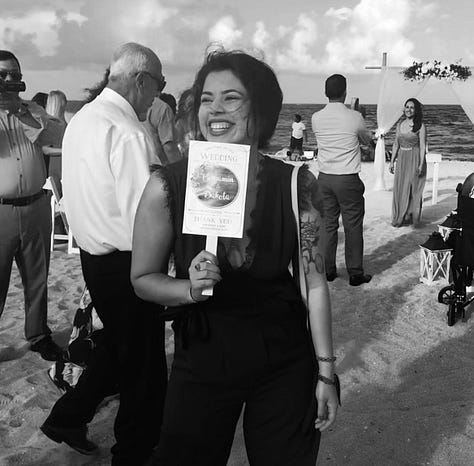
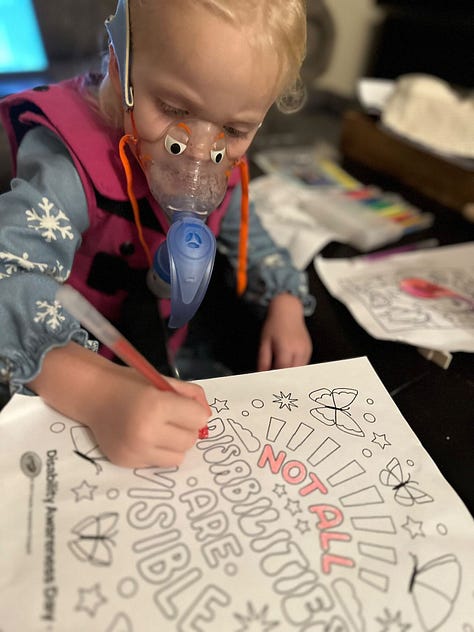
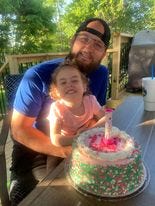
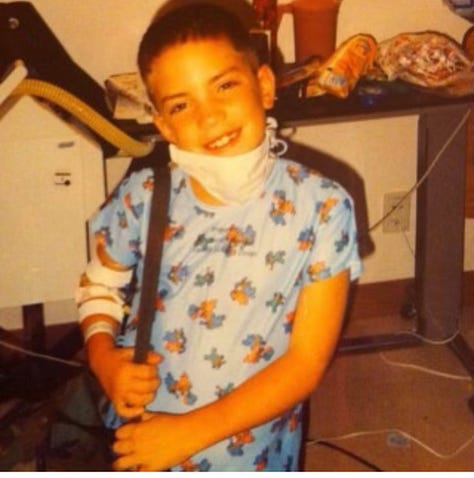
Throughout this essay, you will see nearly fifty different children and adults of the CF community represented from across the United States and from around the world. I’m grateful people decided to share their photos. I love this community and I’m deeply grateful to have so many friends with CF. While I wish none of us had this condition, together we work together to build a better world and future for everybody with CF.
Thanks again for taking the time to be here. No matter if you’re a member of this community or if this is the first time you’ve ever heard of CF, I’m grateful you’re here.









The Point of Awareness Months: On Solidarity
Awareness months have a relatively basic goal: To spread awareness of a problem (or of a condition). But spreading awareness without attempting to resolve said problem can make people feel stuck or confused about how to help. To that end, the point of awareness months has a more complex, multifaceted goal: To make a population of people aware of a problem they’ve never heard of and to invite people who are aware of a problem to become advocates. Advocacy, then, does not have to be going to Congress to advocate to legislators to advance policies (though, we do need that, which I’ll get into later in the essay). Advocacy looks like spreading awareness further, in contributing financial support to organizations who are directly working to resolve the problem, and to doing your part in becoming a better ally to members of a disadvantaged community, which in this case, is the cystic fibrosis population. But (and I’ll be a broken record in saying this, but that’s the point) not everybody with cystic fibrosis is the same. Which then entails a demand for our community to have solidarity across boundaries: racial, sexual, gender, international, mutations, and otherwise.
There are so many conditions that affect so many people so it’s impossible for us to all be advocates all the time for every condition that we hear about. This idea that we should advocate for each problem individually creates internal tension within disease communities as well as external tension between communities with different diseases. It can feel like we’re all competing for a limited amount of capital, or a limited amount of government legislation, or even a limited amount of hearts and minds of potential advocates. This mindset shifts us into an “us vs them” binary whether we realize it or not. Not every disease community has to rely on mutually exclusive baskets of capital, legislation, and advocacy. This is what solidarity and allyship mean to me.
I often position myself as a disability advocate, not because I know what it’s like to have every disability (disability is not homogeneous and every single person’s experience varies), but because we should be advocating however we can whenever we can to improve the world. To not do so while also advocating for ourselves is both morally bankrupt and a betrayal of those we’ve asked to advocate for us. Accessibility looks different to me than it does for somebody with spinal muscular atrophy, just as research into therapeutics looks different between our communities. But both groups would be better supported with improved accommodations and a shared pursuit of genetic therapies. Some disease communities are hard-hit by microbial resistance, but microbial resistance is a threat to everybody, whether you have cystic fibrosis or not. Medical expenses and medical debt affect every person with a disability and affect even more people with transient experiences as they pass through the healthcare system for short-term health problems only to be shadowed for decades by debt. We should prioritize reduction of suffering across every community and we should prioritize opportunities to advocate for collective, broad-facing action.







Solidarity should be one of, if not the top priority for every disease community including the CF community. Perhaps it should be phrased differently: Maybe solidarity shouldn’t be a priority so much as a guiding principle for our efforts. I do believe that most people intuitively understand solidarity, but we should still emphasize its need. In CF, we have flagrant disparities that are arguably worsening with time: Racial and ethnic inequities, those with lower socioeconomic status, people without access to modulators or those who struggle to tolerate them, people outside the United States, those who have received a lung transplant, just to name a few. I don’t believe many are doing this, but we can’t let progress for one community halt our action and advocacy for the remaining communities. We need to increase access to those outside the US without CF, we need to improve outcomes for people with CF in the US, and we need to ensure that we express solidarity (through continued awareness and action) with every other member of our community forever. We need to realize that living with CF does not position us in an entirely different way from somebody with SMA, multiple sclerosis, pulmonary fibrosis, pulmonary hypertension, cancer, or any other condition. In fact, as people who have dealt with the trauma that comes with having a chronic disease that can destroy our quality of life, we can relate to others who have had similar circumstances.









What is cystic fibrosis? How is it treated?
If you’re here, you’re here for one of two reasons: You yourself are already connected with me or somebody with CF, or you’ve somehow stumbled upon this essay through it being an awareness month essay. So if you’re already familiar with CF and want to know more about awareness, advocacy, and how you can get involved, you can feel free to skip this part (though, I believe that we can always become more knowledgeable about CF, which can strengthen our ability to advocate). If you’re not familiar with CF, let’s go through the (non-comprehensive) basics.
Cystic fibrosis is a recessive genetic disease affecting approximately 40,000 Americans, and more than 70,000 people worldwide.
This is just the science-y way of saying that both parents must carry a disease-causing mutation in the specific gene that details the instructions for the cystic fibrosis transmembrane conductance regulator (CFTR) protein.
Recessive means that it’s possible for somebody to carry the gene without having any symptoms (though, and maybe this is too in the weeds for this type of blog, we’ve learned in recent years that carriers do actually experience some clinical problems related to their carrier status).
To inherit CF in traditional terms, a person must have two copies of a disease-causing mutation.
If both parents are carriers, there is a 25% chance that each child will inherit cystic fibrosis. This means that there was a 25% chance Alyssa would inherit CF and then a 25% chance I would. But in statistics, if you’d like to know the likelihood of two independent events both occurring, you multiple those probabilities. In that event, there was a 1-in-16, or 6.25%, chance that Alyssa and I would both have CF.









There are over 2,000 disease-causing mutations.
Not every disease-causing mutation is known; alternatively, not every mutation in the CFTR gene causes CF. This is an important distinction. It’s also important to note that not every mutation causes the same type of defect in the CFTR protein, nor does every person with the same mutations present the same. CF is not a heterogeneous disease.
There are complicating factors here, and again this is probably too in the weeds, but since people must inherit two disease-causing mutations, some people have two different mutations while many have the same mutation on both chromosomes they inherited from their parents. Additionally, our DNA, genes, and proteins of course do not exist in a vacuum. Some genetic factors can worsen CF health, while some can actually help ameliorate some of the impacts of the defective CFTR protein. Our environment also plays a large role. This is why factors like pollution, climate change, diet and nutrition, exercise, and more are major research priorities in the world of CF.
Many people call CF a lung disease, but this flattens the complexity of the condition and undermines the more serious implications. Cystic fibrosis is ultimately a disease that disrupts our body’s ability to transport salt and water across cellular walls. This is most typically presented in how it disrupts our body’s ability to create mucus. Mucus is an essential part of our body’s defense, but too thick of mucus is a problem. With defective CFTR protein (and again, different mutations result in different defects in the CFTR protein), salt and water are not transported adequately to the mucus, thus preventing the mucus from becoming more fluid. Excessively viscous mucus then impedes the body’s defense against intruders including pathogens and environmental particles. There is a lot more to this, but thick mucus is a perfect breeding ground for bacteria, leading to CF lungs often cultivating thriving bacterial ecosystems for decades. The thick mucus is also too thick for tiny hair-like cells called cilia to appropriately clear out the mucus.
Simply: Both infection and inflammation are major issues for people with CF, especially in the organs where mucus plays a major role. That includes the lungs, gastrointestinal tract, pancreas, sinuses, and reproductive tract. But many people with CF also have problems with their kidneys, liver, skeletal system, and more. CF is a beast of a disease.









Every person with cystic fibrosis has different varying manifestations of CF, so treatment regimens can look different for most people. It’s possible for people to have the same regimen, but it’s not appropriate to view any treatment as one-size-fits-all.
I want to be very clear: This is not exhaustive! This is intended to give an overview of many aspects of life with CF, not comprehensively capture every circumstance. This is just one reason awareness months are important: To ensure we are amplifying the stories of people across the spectrum. I’ve included links to the CF Foundation’s pages on the various treatments to ensure people can access more in-depth information.
Many people with CF are pancreatic insufficient, meaning our pancreas doesn’t produce enough of the compounds that break down food, which are known as enzymes. Pancreatic insufficiency is generally caused by thick mucus (this will be a theme). Many of us have had to take enzymes before we consume food and drinks for our entire lives. And a question we often get from people without CF is, “What would happen if I took those?” I’m not too sure, but let’s not experiment.



Again, mucus is a theme. Since people with CF have thick mucus in their lungs, mucus holes up in our large and small airways, causing the problems that can wreak havoc on us for decades. As one part of what is usually a regimen with multiple therapies, people with CF perform (or have performed) chest physiotherapy. There are a couple different types of airway clearance techniques, but high-frequency chest wall oscillation is the one most people have seen before (the Vest or Monarch).
For the old heads, we remember receiving airway clearance from our parents or caregivers. In my family, we called them “poundies.” Life with CF can be many things, but strange is definitely one of them.
Inhaled medications
Hypertonic saline
Pulmozyme
Mannitol
Not all antibiotics are inhaled and for more severe exacerbations (which are flare-ups in CF lingo), intravenous antibiotics are usually used if oral antibiotics aren’t effective.








Inflammation is the second major beast in the CF world after infection. But inflammation is a challenge for different reasons. It’s hard to argue that an infection is ever a good thing, but inflammation is actually a good, healthy physiological response. Too much inflammation, though, is not, and that’s the problem for many people with CF.
And then, the drugs that have become the poster child of medical and scientific advancement: modulators. There are four currently-approved modulators (Kalydeco, Orkambi, Symdeko, and Trikafta) with more in development across various stages of the clinical trial process.
Modulators are remarkable because they have shown that it’s possible to significantly restore CFTR function without gene therapy, a revelation that only became known about a decade ago when Kalydeco was approved for people with the G551D mutation. For years, it was unknown if modulators would be able to restore more complex mutations like ∆F508, the most common mutation. Then Trikafta revealed that ∆F508 could see a similar restoration of CFTR. I won’t get into the more intricate minutiae, but I mentioned above that mutations can cause different problems with the CFTR protein; this is why not every patient is eligible for modulators and why not every modulator works as effectively for everybody. CF is a complex disease!
Modulators are a challenge to discuss. For many people, including myself, Trikafta has been profoundly life-altering. It has sustained me in ways I hadn’t known for decades; I’ve managed to reduce my burden of care significantly, coming off many of the therapies I mentioned above; infections (including viral) are much more manageable. But for others who’ve tried modulators, they’ve either not benefited much or at all or experienced adverse effects that reduce their quality of life; and still, for others, they aren’t even eligible for these potentially life-altering therapies, either because they do not work for their mutations, or because they live in a country that does not have access to them. Again, this why we need solidarity and international cooperation.
Organ transplants
I would be remiss if I didn’t discuss lung transplants which, though they have become less common in the era of modulators, still remain a major hurdle we need to drive progress forward on. Lung transplants are not guarantees of success, as my sister’s story attests, with many people still facing significant quality of life challenges and shortened life expectancies. This is just another reason why solidarity among our many subcommunities is crucial; many feel that once they receive a lung transplant, since their treatment plan radically changes, they aren’t quite as part of the CF community as they once were. When somebody receives a lung transplant, they become members of a new community of people who need solidarity, advocacy, and progress. We must advocate for this community too, not only because they are members of the CF community, but because we need to remember that we must advocate for one another, always.









The Future of CF: The Path to a Cure and the Infection Research Initiative
There are many exciting things happening in the CF world right now. First, there’s the Path to a Cure, the CFF’s commitment to invest in multiple different approaches to give rise to a cure. I would love to cover the full extent of the Path to a Cure initiative, but I worry that this would detract from the essence of the essay and get too into the science. Please check out the CFF’s page on Path to a Cure to learn more.
Another note, just to convey the complexity of these therapies: Gene therapy doesn’t technically capture the scope of the future potential therapies, as there are other approaches including RNA therapy and gene editing, but I’m using this term more generally for simplicity.
Modern science and medicine have us thinking more about a cure than we’ve ever truly considered before. Cellular and gene therapy are not the future; they’re already here. Clinical trials are beginning for the cystic fibrosis community. I suspect we will see a groundbreaking therapy within a decade, if not sooner. I can’t express the urgency here because gene therapy offers a holistic possibility for our community: a mutation-agnostic possibility that gives hope to everybody in our community, modulator-eligible or not. For those who have not yet been able to access the potential from a modulator like Trikafta, this reality is of the utmost importance.
But there’s something here that we as advocates who must commit to solidarity across the entirety of our community mustn’t forget: We cannot see a world where gene therapy is only available to those of us in the wealthiest nations. CF is a disease that affects people across the world, and as we witness worsening inequity, we cannot see a cure or groundbreaking therapy in one part of the world while others don’t have access to therapies that I and other Americans have had access to for decades.
There’s also the CFF’s (now over) $100 million Infection Research Initiative, which is exploring potential innovative approaches, including phage therapy, to combat infections.









Congressional actions of particular importance to our community
I have pulled information from the Cystic Fibrosis Foundation on these Congressional actions, including how you can help try to get these passed. In the spirit of action in addition to advocacy, I am asking you to support the legislative actions below.
Organizations Focused on Fight Against Superbugs Celebrate Reintroduction of the PASTEUR Act
From the CFF:
Congress has reintroduced the PASTEUR Act to bring new antibiotics into the hands of those who need them most. Now it’s our turn: urge your members of Congress to pass this bill without delay.
Despite significant progress in treating cystic fibrosis, infections remain a serious threat to the health of people living with the disease, and many rely on antibiotics as part of their regular treatment regimen. But with antibiotic-resistant infections on the rise and few drugmakers investing in research or development to bring new options to market, there simply aren’t enough antibiotics available to meet the challenges that lie ahead.
The PASTEUR Act is a critical step forward in our efforts to address the antimicrobial resistance crisis. This bipartisan bill will incentivize the development of urgently needed antibiotics and antifungals while implementing standards to use these critical medications more efficiently.
The CF community was instrumental in driving the PASTEUR Act forward in the last Congress – and we aren’t done yet. Your stories are essential and will be the reason why we make it over the finish line to pass PASTEUR this year.
CF Foundation Applauds Reintroduction of the HELP Copays Act
From the CFF:
Transformative therapies — such as CFTR modulators — have been paramount in shifting what it means to live with cystic fibrosis. The Cystic Fibrosis Foundation recognizes the challenges insurers face in managing the rising cost of drugs often associated with these life-changing therapies. However, cost containment strategies instituted by insurers, such as accumulator and maximizer programs, or the decision not to cover a high-priced medication altogether, unfairly place patients in the middle of a fight that belongs between insurers, manufacturers, and pharmacy benefit managers.
The Foundation applauds the reintroduction of the HELP Copays Act — bipartisan legislation that helps patients access necessary prescription drugs by potentially reducing the financial burden that results from complex and hard-to-navigate health insurance plans.
Living with a rare disease such as cystic fibrosis is costly enough. Adding complex and unwieldy complications to health insurance plans exacerbates an already unimaginable reality of financial constraint that could result in irreparable harm to patients and families. While a short-term fix to a systemic issue, the HELP Copays Act will protect patients and their families from having to sacrifice their health when they cannot afford necessary, life-changing prescription drugs.








No Work Requirements in Debt Ceiling Package
From the CFF:
Congress is negotiating to raise the debt limit and is considering a deal that would implement work requirements as a condition of eligibility for key programs like Medicaid and the Supplemental Nutrition Assistance Program (SNAP). This proposal would be harmful to people living with CF and we must speak out. While many in the CF community can and do work, their ability to do so can vary over time. Programs like Medicaid and SNAP help many people with CF manage their health, and the ability to work should not be a barrier in accessing those vital resources. All people with CF must be able to access the high-quality, specialized care they need to live longer, healthier lives. Work requirements will significantly hinder that access.”
CF Foundation Advocates to Protect Needs of People With CF in Post-Pandemic Medicaid Redeterminations
From the CFF:
Medicaid has long been a crucial source of health coverage for many people living with cystic fibrosis, often filling gaps left by private insurance; roughly half of all children and one-third of adults with CF in the U.S. rely on Medicaid for some or all their health care coverage. During the COVID-19 pandemic and its economic impact, the program played an especially vital role in helping people with CF afford the specialized care they need to stay healthy. Now, with states beginning to resume disenrollments, the CF Foundation is taking steps to ensure impacted people with CF do not lose their coverage.
If you utilize Medicaid, be sure your contact information with Medicaid is updated and promptly reply to any communication you receive from your state. Individuals may be disenrolled due to changes in residency, income, age, or lack of information substantiating eligibility.
If you need assistance, our case managers can review your insurance options and help you make the transition to new insurance. Connect with CF Foundation Compass by calling 844-COMPASS (844-266-7277), emailing compass@cff.org, or submitting an online request form.









Organizations you can support
Emily’s Entourage, whose mission is to “accelerate research and drug development for the final 10% of people with cystic fibrosis (CF), including those with nonsense mutations.”
The National Organization of African Americans with Cystic Fibrosis (NOAACF)
Cystic Fibrosis Research Institute (CFRI), whose mission is “to be a global resource for the cystic fibrosis community while pursuing a cure through research, education, advocacy, and support.”
CF Roundtable, a quarterly publication led by a community of adults with CF.
Rock CF, “a community thousands strong changing the face of what living with Cystic Fibrosis looks like and giving those living with CF the tools to not only survive, but thrive”
Please let me know if I missed any that you think I should include. I would be happy to add to this list.








A message to those we’ve lost along the way
This essay would not be complete without acknowledging that we have lost countless people to CF so far. Generations of people did not get a chance to live the lives they deserved, free from the suffering that comes with CF. Many did not get a chance to see adulthood, or any semblance of a healthy adolescence; many did not get a chance to travel, to marry, to have children, to live for even a short time with stable health. We can’t — and won’t — forget these stories. We carry on because we have no choice but to carry on and build a better world. We will continue to tell their stories because to grieve is to have loved.








Conclusion
Thanks for taking the time to read this. I hope you’ve learned something, whether you have CF, are already involved in CF research, or if you’re just learning about it today. I ask that you share this post as a basic gesture of action in the spirit of awareness and to do your part in being an ally to our community, whether that’s in supporting legislation, donating to the CFF (or starting a Great Strides team), or in supporting people with CF or other disabilities by working to be a more inclusive colleague. Whatever you choose to do, it will make a difference.
Until it’s done,
Tré









And a special thank you to the global community of people with CF who shared their photos for this essay
Aimee (she/her), 38, Utah; Alexie (she/her), 22, Ontario, CA; Ally (she/her), 28, Missouri; Alyssa (she/her), 29, Kentucky; Andrew (he/him), 9, Lexington, KY; Andy (he/him), 49, Georgia; Annabelle (she/her), 24, Surrey, United Kingdom; Ariella (she/her), 25, Tennessee; Caleigh (she/her), 32, California; Cameron (he/him), 29, Kentucky; Camille (she/her), 27, Utah; CeCe (she/her), 5, Lexington, KY; Chelsea (she/her), 34, Montreal, Canada; Claire; Ella (she/her), 31, Virginia; Emily (she/her), 38, Ardmore, Pennsylvania; Emily (she/her), 41, Michigan; Gabby (she/her), 26, California; Gillian (she/her), 31, Indiana; Heidi (she/her), 31, Kentucky; James (he/him), 36, Huntsville, Alabama; Jen (she/her), 52, Durham, North Carolina; Jenny (she/her), 35, Utah; Julia (she/her), 30, Texas; Kareem (he/him), 6, Lebanon; Kathy (she/her), 60, Eugene, Oregon; Katie (she/her), 41, Virginia; Ken (he/him), 31, Massachusetts; Kira, 23, Florida; Kylie (she/her), 22, Kentucky; Luisa (she/her), 29, Tennessee; Lynnie (she/her), 3, Kentucky; Makenzie (she/her), 25, Kansas; Marissa (she/her), 46, Louisiana; Morgen (she/her), 26, Florida; Natalie (she/her), 26, Washington; Noor (she/her), 33, Boston; Rylee (she/her), 4, Kentucky; Sofia (she/her), 2, São Paolo, Brazil; Steve (he/him), 71, Minnesota; Sophia (she/her), 32, Grand Rapids, Michigan; Taylor (she/her), 27, West Virginia; Tré (he/him), 29, Arlington, Virginia; Trey (he/him), 4, Maryland; Will (he/him), 26, Chicago, Illinois; Xan (they/them), 39, Florida; Yazar (he/him), 30, Jordan.




So much amazing information!